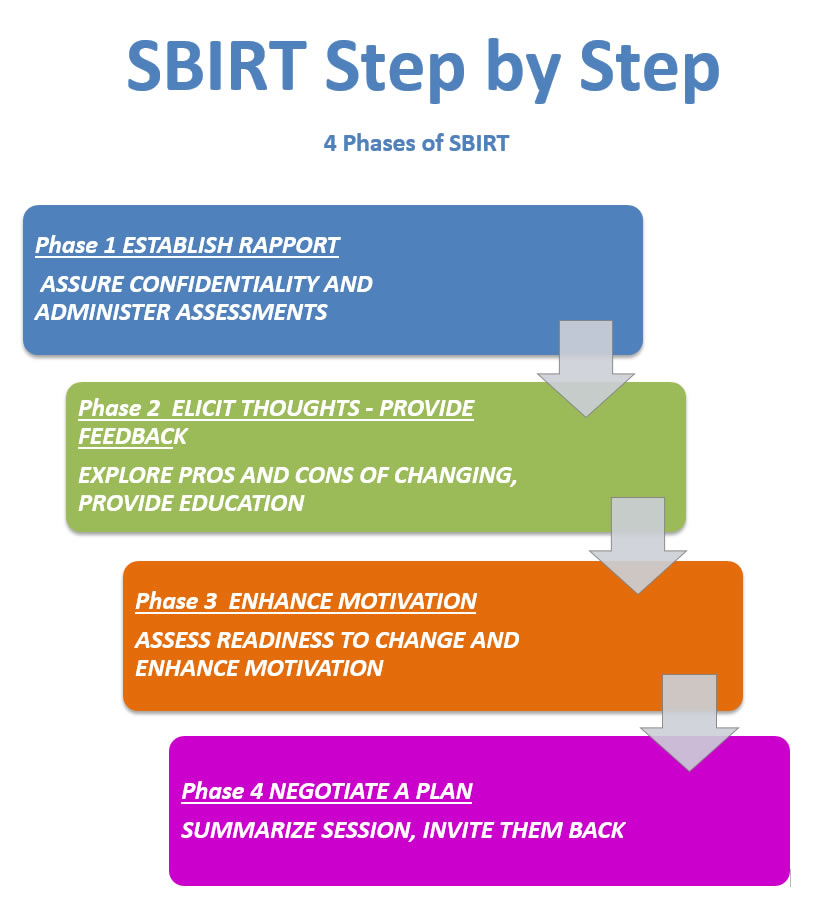
Steps of a Brief Intervention
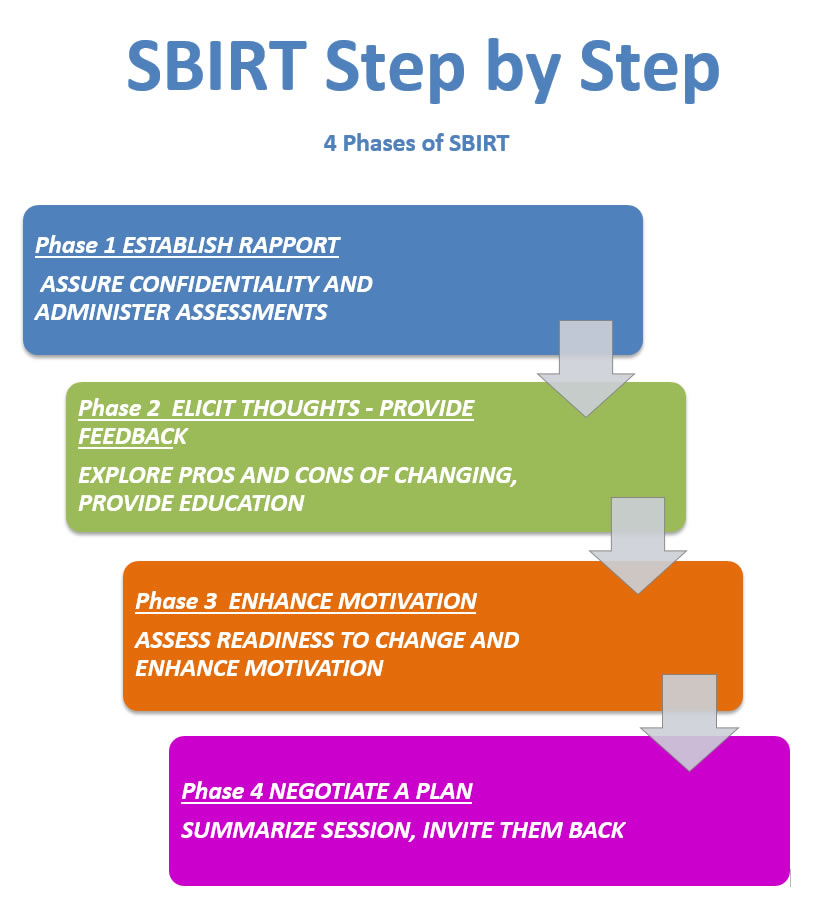
THE PHASES OF SBIRT
Example of a SBIRT Conversation
Phase 1
ESTABLISH RAPPORT AND ADMINISTER ASSESSMENTS
Hello Mr. /Mrs. /Ms. (last name or other formal name). My name is ________
I am part of your care team here at _________. We are now talking to each patient, no matter why they are here, about their alcohol and drug use, and about depression. We know that these things can have a significant impact on your health, and we care about your health. Is it all right if I ask you some questions?
Assure confidentiality
Everything you tell me is completely confidential and will be shared only with your health care providers here at this clinic. Do you have any questions or concerns?
Administer assessments
Phase 2
ELICIT THEIR THOUGHTS
PROVIDE FEEDBACK AND EDUCATION
Discuss results
Your responses to these questions go along with what you've told me. Your scores indicate that you are (summarize the results). What are your thoughts about this?
Explore the pros and cons and develop discrepancy
What are the good things for you about X? (… is there anything else?)
What are the not-so-good things about X? (… anything else?)
So on the one hand…… and on the other hand….
What do you know about the way ___________(substance) effects your body?
What concerns related to your health do you have when you think about the effects?
Sounds like you already know how ____________ causes ___________. (Expand their statement and perhaps add if it applies).
Would it be ok with you if I shared some information with you about how (specific substance use) can affect your … (i.e., whatever is relevant to the patient, e.g., mood, breathing, diabetes, etc).
Determine how much health information/education will help motivate the person given their stage of change, e.g., for pre-contemplation or contemplation stages, patients may benefit from a more general and brief presentation of risk; use of brochures may or may not be apropriate at this point.
Any thoughts? Concerns? Any particular area that you see that relates to you or your life right now?
Phase 3
ASSESS AND ENHANCE MOTIVATION USING THE READINESS RULER
Show the Readiness Ruler
On a scale from 0 to 10, with 0 being not at all ready to change and 10 being very ready to change, how ready are you to make any change at all (even a small one) in your substance use?
What motivates patient and what are the barriers?
Why that number and not XX (lower number)? (Change talk)
Why that number and not XX (higher number)? (Barriers for change)
So on the one hand A and on the other hand B… (E.g., “So on the one hand alcohol relaxes you at night, but on the other hand it makes it hard for you to get up on time in the morning. Do I have that right?”)
Explore patient’s ideas about implementing change
What steps, if any, might you take from here?
If patient is not interested in changing (pre-contemplator), increase perception of risk and problems with current behavior.
If I understand you correctly, you know the health risks and the problems it causes, but you’ve decided to take your chances and stick with what you are doing for now. That’s fine-- it’s your choice. I just want to be sure you have all the information you need to make decisions.
Is there anything you can think of that might come up or change in the future that would make you want to make a change?
Is there a down-side to having things stay the way they are?
Validate that patient isn’t ready to change and acknowledge their control of the decision.
I hear you saying that you are nowhere near ready to change. You are the one to decide if and when you are ready to make a change.
If patient is aware that a problem exists and is considering action, but has not yet made a commitment to change (Contemplator):
So it sounds like you are having some problems with … and (say negative effects of it) and you think that if….. (you changed something) things might improve. Is that right?
Gather information about past change attempts, and frame in terms of some success rather than failure. Affirm the patient’s attempt to change.
Have you ever tried to change in the past? What did you do? What was helpful? So, despite the challenges, you took action and (summarize patient’s attempt and what worked).
Build on past success/effort and explore additional options for change.
What would you like to have happen now?
What might you do differently now?
Phase 4
NEGOTIATE A PLAN, SUMMARIZE AND END ON A POSITIVE NOTE
If patient is ready to make a change (Preparation), praise the decision to change behavior! Assist patient in building an action plan. Examine barriers and elicit solutions. Build coping behaviors
Is there one thing you might be willing to change right now?
How do you plan to do that?
TIPS for Setting Goals
Can you think of one thing you could do to make a change in the next month?
Never mind the “how” for right now. What would you like to achieve?
So what do you intend to do?
What strengths do you have that will help you succeed?
Who could offer you helpful support in making this change?
How confident are you that you can make this change?
Do you see any barriers to making this change? What are they? What can you do to overcome them?
What will happen if you slip up?
Can you write it down here in your own words?
(Hand them an informational brochure-- on the back is a space to write a goal/plan)
For patients whose AUDIT and/or DAST results indicate a BT or RT:
BT
We offer counseling services here at our clinic that may help you achieve the changes you want to make. You can meet with me at no cost, or with one of our clinic counselors. What do you think?
RT
Given everything we’ve discussed, I think it would be helpful for you to take advantage of a program that specializes in ……. What do you think?
Emphasize door is always open
Thank you for talking with me today. I appreciate your time, and your honesty in talking with me.
Please let me know if there is anything I can do in the future to help you in any way.
The door is always open to talk with me or your health care staff.